Advertisement
I Tried A Low-FODMAP Diet & It Actually Healed My Gut
Five years ago, I came down with what I thought was a stomach bug or a bout of food poisoning—loss of appetite, nausea, fever—that stuck me in bed for three or four days. I didn't eat much over this time but didn't think I was dealing with anything extreme. Finally, my appetite came back, but as soon as I reintroduced food into my system, I couldn't eat anything without experiencing diarrhea afterward.
I was afraid to eat anything other than oatmeal and scrambled eggs, as those were the only foods that didn't send me running to the bathroom. As a foodie who's always thinking about what I want to cook next, this was incredibly frustrating and upsetting.
To add to this stress, I was working in my first real office job at the time. I didn't want my discomfort to ruin my workday, which of course, it did. My "fix" at work came down to barely eating so I could prevent discomfort. This resulted in unhealthy weight loss and a feeling of total isolation. I didn't feel comfortable going out to eat with my friends or even having coffee with my co-workers.
Finally, after a lot of concern from not only myself but my family, I visited a GI doctor. I went through the as-fun-as-you-can-imagine stool test, but results came back inconclusive for any specific infection (as I had waited to see a doctor), nor did it come back with any indication of other serious problems.
He saw my lack of relief and said that the best way to describe what happened was that I came down with a GI infection like gastroenteritis, which resulted in me developing irritable bowel syndrome. Specifically, based on my most severe symptoms—pain and diarrhea—he said that the infection affected the nerves around my gut, affecting motility and sensation. Furthermore, my microbiome was most likely severely depleted, as my food was moving too quickly through my system, preventing proper digestion and absorption.
I was lucky enough to find a GI doctor who had a dietitian on staff. She reviewed the doctor's notes about my tests and subsequent infection diagnosis. During my first visit, she had me write down everything I had eaten the day before. She looked at my diary, asked me how I felt after eating these foods, and when she heard my response, she knew immediately what I needed to do.
"Have you ever heard of FODMAP foods?" she asked. I had not (and keep in mind, I have a dietetics and nutrition degree).
That was the beginning of my deep dive into the low-FODMAP lifestyle.
FODMAP is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. Basically, they're types of sugars found in different foods at different levels and can cause discomfort during digestion for those people who have compromised gut function.
I learned that fructose, a simple sugar or monosaccharide, is a sugar I react to most. Fructose is usually digested and absorbed in the small intestine. If properly digested and absorbed, the broken-down fructose molecules travel into the bloodstream to the liver for metabolizing. If you have trouble digesting fructose, though, the fructose travels farther down the GI tract and becomes the perfect food for bacteria to consume, causing gas, bloating, and pain. Additionally, excess fructose consumption can draw too much water into the intestines, causing diarrhea.
Fructose is found in many of the foods and drinks I used to love to consume—apples, protein bars, green juices—just to name a few. All of these foods end up on the FODMAP "do not eat" list, which I'll get to in a bit.
Finding this out was overwhelming. But I knew that I couldn't go on any longer feeling bloated, fatigued, and in pain. Enough was enough.
I began my new plan to eliminate high-FODMAP foods from my diet, along with other lifestyle changes.
The biggest culprits in my own diet, and the most difficult to cut out, included apples, honey, stone fruit, agave, garlic, onions, wheat products, and cashews. Unfortunately, I had to cut these foods out entirely, in true elimination-diet-style. I needed to start taking a quality probiotic to rebuild my gut flora, educating myself on reading food labels more carefully for hidden sugar terms and getting more comfortable asking questions when dining out.
I'm not going to sugarcoat it…at first, it really sucked. I knew that in order for this to work and to feel better, I needed to be strict, which meant cooking most of my meals at home and scrutinizing food labels.
It's been over five years, and it's been quite a journey. I struggled, especially in the beginning, relearning what I knew about how to feed and nourish myself.
Here are six things I've learned on my low-FODMAP journey:
1. Get familiar with the lists of approved/unapproved FODMAP foods.
I kept a list on my phone and also downloaded the Monash University FODMAP app. Monash University revolutionized the understanding of IBS through a major study of how dietary treatment can help manage IBS. The more you look at this list, the easier it will be to recognize foods (and even full meals) that may cause discomfort. Additionally, when you're out at a restaurant, which I often am, I know I can refer to this list if there's ever a question about a particular dish.
2. Learn how to better analyze food labels.
I used to eat a packaged protein bar every day and didn't realize that one of the main ingredients was inulin, a prebiotic fiber that also happens to be an oligosaccharide (the "O" in FODMAP). Prebiotics are great for gut health but not when you're unable to digest FODMAPs, which can cause major gut distress. Learn how to spot hidden sugars on food labels—the food industry loves feeding us sugar, even when they're touting a product as "healthy"!

3. Try an elimination-style diet (under the supervision of a health care practitioner).
In order to truly understand what FODMAP foods upset my system most, I needed to cut them out and then reintroduce them. I hated having to cut out garlic and onion—I love cooking Italian food—but it's a temporary diet to determine which foods you can handle in certain quantities. There are some foods you may find you can never have in large quantities, but trust me, if that Honeycrisp apple makes you gassy and bloated afterward (*raises hand*), skip it and send a little love from afar when you pass 'em at the farmers market.
4. Supercharge your gut-healing with a quality probiotic.
I needed to start taking a daily probiotic, but there are so many different kinds on the market, it was tough to find the perfect one without help. Jessica Cording, M.S., R.D., CDN, recommends choosing probiotics with multiple strains in order to promote a well-functioning digestive system, help the body absorb and utilize nutrients, and regulate serum cholesterol. With the help of my dietician and naturopathic doctor, I found a probiotic that really made a difference in my digestion, full of different types of Lactobacillus and Bifidobacterium bacterial species. Looking for more help choosing the best type of probiotic for your needs? Check out this super-comprehensive piece from gut-health specialist Vincent Pedre, M.D.
Cording's main recommendation when working to heal your gut? "You need to be mindful to continuously replenish and repopulate your system with these guys, whether it's through food sources, supplements, or both," she says. "It's also important to include foods that are a good source of prebiotic fibers that can act as nourishment for probiotic bacteria."
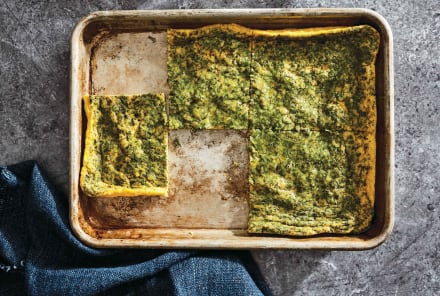
To this tune, I worked to add probiotic foods to my diet such as kombucha, pickled vegetables, and kefir (nondairy, as I am also lactose-intolerant!), as well as low-FODMAP prebiotic foods such as bananas, oats, and greens.
5. Figure out ways to make the diet easier for you.
I work full-time in a job that I love, spend a lot of time with friends and family, and often go to a workout class before or after work. With my busy schedule, sometimes cooking is just not in the cards during the workweek.
While there aren't a ton of companies around that cater to low-FODMAP eaters, there are a few great ones, and they've been a huge help in fitting the diet into my busy lifestyle. Epicured, a meal-delivery service, is led by a team of IBS-management experts, including a registered dietitian who helps patients with IBS daily, with recipes developed by Michelin-star chefs. I love their Tofu Pad Thai, Zucchini "Spaghetti" Bolognese for a high-protein dinner after a HIIT workout, and their Vanilla Coconut Chia Pudding With Raspberries for a seemingly decadent, high-fiber breakfast to bring to work.
With garlic on the no-go list for low-FODMAP eaters, making good Italian food can be tricky. I love Italian food, and I'm obsessed with Fody Foods "Top Notch" Tomato Basil Pasta Sauce and Garlic-Infused Extra-Virgin Olive Oil. Whipping up some fresh pasta, topped with veggies cooked in their garlic-infused olive oil and then tossed in sauce is now a favorite, delicious weeknight meal option.
For my daily protein bar, I now reach for Fody Foods Dark Chocolate Nuts & Sea Salt bars (it tastes like a Snickers bar, and I'm not mad about it) and GoMacro bars, especially their Peanut Butter Chocolate Chip and Sunflower Butter & Chocolate flavors. These kinds of bars make great travel snacks (I hate buying airport food) and are perfect to stash in my desk for an afternoon pick-me-up.
6. Figure out what's temporary and what should be permanent.
As I mentioned before, the low-FODMAP-style elimination diet is meant to be temporary, so I've added foods back into my diet that I can handle in smaller amounts—garlic, onion, cashews, and legumes—and I've kept foods out that I can't handle—apples, honey, agave, and stone fruit.
I do still experience the occasional symptoms of my IBS, such as pain and diarrhea, so I continue to take my daily probiotic, and I'm wary of how much fructose I'm consuming. But, I've dived back in to my favorite food activities, exploring NYC restaurants and cooking at home.
Whether this is the beginning of your healing journey, you're somewhere in the middle, or you're like me, maintaining your new normal...be patient and kind with yourself. You may have great days, and you may have really bad days. Dealing with chronic digestive issues can take an emotional and physical toll, so it's most important to learn how to listen to your gut, in all senses of the phrase.
Watch Next
Enjoy some of our favorite clips from classes
Enjoy some of our favorite clips from classes
What Is Meditation?
Mindfulness/Spirituality | Light Watkins
Box Breathing
Mindfulness/Spirituality | Gwen Dittmar
What Breathwork Can Address
Mindfulness/Spirituality | Gwen Dittmar
The 8 Limbs of Yoga - What is Asana?
Yoga | Caley Alyssa
Two Standing Postures to Open Up Tight Hips
Yoga | Caley Alyssa
How Plants Can Optimize Athletic Performance
Nutrition | Rich Roll
What to Eat Before a Workout
Nutrition | Rich Roll
How Ayurveda Helps Us Navigate Modern Life
Nutrition | Sahara Rose
Messages About Love & Relationships
Love & Relationships | Esther Perel
Love Languages
Love & Relationships | Esther Perel
What Is Meditation?
Box Breathing
What Breathwork Can Address
The 8 Limbs of Yoga - What is Asana?
Two Standing Postures to Open Up Tight Hips
How Plants Can Optimize Athletic Performance
What to Eat Before a Workout
How Ayurveda Helps Us Navigate Modern Life
Messages About Love & Relationships
Love Languages
Advertisement

How To Use Food To Recover From Autoimmunity: An MD's Top 4 Tips
Sara Szal Gottfried, M.D.